As a health information technician, you will be a member of the allied health team specifically trained in the technical areas of health information. These areas include the collection, analysis, dissemination, and maintenance of health care and patient-related data including medical records. Health information technicians are also trained in basic management and supervisory principles for health information services, quality improvement and utilization management.
The Health Information Technology program at Onondaga will prepare you in the areas of:
- Basic information principles.
- Numbering, filing, storage and retrieval systems in health care information.
- Review of the health care record for accuracy and completeness.
- Computer applications in health information management.
- Legal aspects of maintaining and releasing health care information.
- Health care legislation and its impact on health information services.
- Standardized coding procedures.
- Case-mix groups and other reimbursement systems.
- Utilization management.
- Risk management.
- Corporate compliance.
- Quality and performance improvement and peer review functions.
- Management and supervisory issues in health information services.
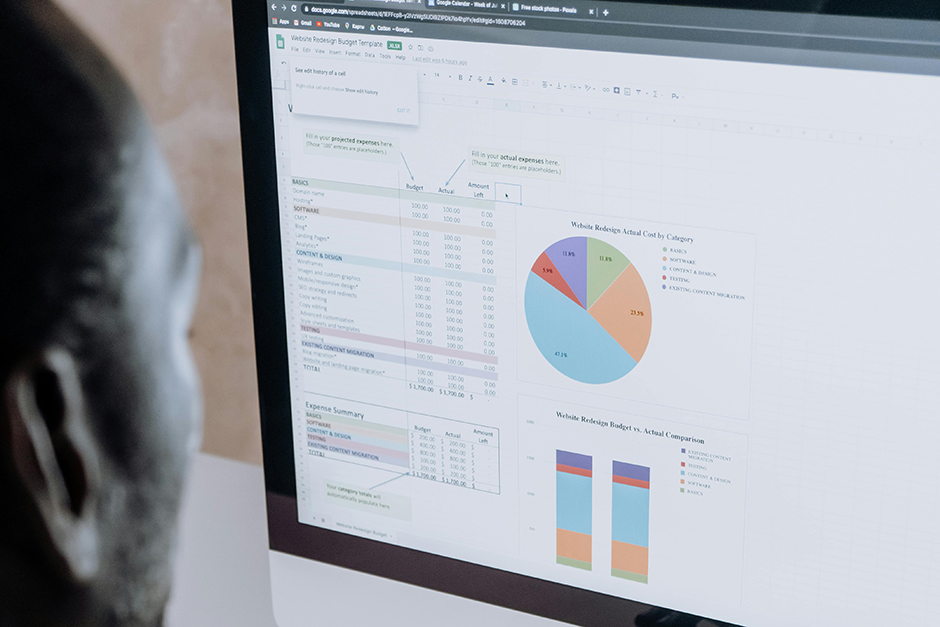
- Analysis and display of health care data.
- Maintaining requirements/standards for accrediting and certifying agencies.
- Calculating and displaying health care statistics.
Employment opportunities continue to expand in ambulatory care, long-term care, home care, HMOs, psychiatric facilities, industrial clinics, physicians’ offices, law offices, insurance companies, sales of health-related products and services, residential care, and state and federal health agencies as well as a number of other areas.
Professional Practice
The Health Information Technology program at Onondaga will allow you to put classroom theory into actual practice through professional practice courses. You will be required to complete two clinical practicums.
Professional Practice Experience I, for one credit hour, is taken in the second semester and consists of placements in a minimum of five clinical sites for a total of 40 hours.
Professional Practice Experience II, for three credit hours, is taken in the final semester. This involves spending three weeks, full time, at a clinical site gaining experience in the basic technical aspects of health information services.
Students will be required to submit documentation of a current physical examination, PPD, titers and immunizations prior to being placed in a clinical site. Additional expenses may be incurred during clinical practicums due to the need for transportation, parking and proper work attire. Such expenses are the student’s responsibility.
Admissions Requirements
The following requirements must be met before you can be considered for admission to the HIT program:
- A high school diploma or equivalent.
- One year of high school algebra or MAT 087 (noncredit) at Onondaga.
- One year of high school biology or one semester of college biology.
- Grade of C or better for all required courses used to meet admission requirements.
Program
The A.A.S. degree in Health Information Technology emphasizes concentrated studies in health information supported by clinical experiences in cooperating health care facilities and agencies. The HIT program is accredited by the Commission on Accreditation for Health Informatics and Information Management Education (CAHIIM), 233 North Michigan Avenue, Suite 2150, Chicago, IL 60601, telephone (312) 233-1183. Graduates qualify for certification in the health information technology field by passing the national credentialing examination required by AHIMA. Graduates may transfer to a four-year college to pursue a baccalaureate degree in health information management.
Graduation Requirements
BIO 171 , BIO 172 , BIO 221 and all required HIT courses completed with a C+ or higher.
Program Learning Outcomes
- Review and verify health records for timeliness, accuracy, appropriateness, and completeness of health care.
- Apply legal policies, regulations, standards and procedures for the management and control of the patient record, and disclosure of protected health information.
- Perform work processes that support clinical classification and coding.
- Code, abstract, classify and index diagnoses and procedures for the purpose of reimbursement, standardization, retrieval and statistical analysis.
- Review, abstract, retrieve, and compile health data for reimbursement, quality assessment, patient research, clinical registries and other information needs.
- Apply management principles and tools used to effectively manage human, financial, IT and physical resources.
- Apply quality improvement tools and techniques in support of performance improvement initiatives.